In 1951, Lorenz and Jacobsen showed that mice that had received lethal irradiation could be saved with bone marrow collected before the irradiation. These results were the background to Donall Thomas’ attempt to transplant bone marrow from normal donors to patients with advanced cancer after previous total body irradiation. The bone marrow of the patients was replaced by the bone marrow supplied. Markers showed that white and red blood cells in the blood of the recipient were produced by the donor bone marrow. The principle that bone marrow could be transferred from a donor to a patient, that it could grow where the patient’s own bone marrow cells had previously existed and that it could give rise to new red and white blood cells was proven. Anemia due to damaged bone marrow became the obvious indication for continued bone marrow transplantation trials. Georges Mathé in Paris transferred bone marrow to patients after a nuclear accident and Bob Good treated a patient with combined immunodeficiency and aplastic anemia, a disease where the bone marrow is severely damaged. The patient of Bob Good became the first one to be cured. At about the same time, Donall Thomas performed bone marrow transplants of patients with acute leukemia who had recurrence of disease after conventional treatment. These patients almost always died after a short period of time regardless of the continued treatment. In 1977, the results were published in the journal Blood. Thirteen of 100 transplanted patients had apparently been cured from leukemia with bone marrow transplantation. The conditions for starting a bone marrow transplant program were significantly better at the Huddinge Hospital than at the Karolinska Hospital. Curt Franksson had received the professorship in surgery. He was a Swedish pioneer in transplant surgery and had made the first kidney transplant in Sweden. I had also heard that he had succeeded in persuading Carl-Gustav Groth, who was in Denver, USA, to return to Sweden to lead the transplant operation here. An immunological laboratory for matching transplant donors and recipients with Erna Möller as director was to be built up.

Carl-Gustaf Groth had now become head of transplantation surgery at Huddinge and I still remember when I was standing outside the lifts in the corridor at the Department of Medicine and by chance met Carl-Gustav (we did not know each other well then). I said en passant “I absolutely think we should start a bone marrow transplant program at Huddinge Hospital. It is not exactly surgery but would you be interested in a collaboration? ”. I do not remember exactly what response I received but it was essentially very positive.
Our first patient was a 16-year-old boy who was diagnosed with severe aplastic anemia a little less than a year earlier. He had a pronounced bleeding tendency, severe anemia despite transfusions and the number of platelets was well below the levels usually associated with very serious bleeding. His white blood cells were very few and his bone marrow was virtually eliminated. His illness was thus life-threatening. He had a brother who fit immunologically, and they had the same HLA (human leukocyte antigen) pattern – a prerequisite for transplantation at all. The patient was admitted to the hematology section on October 13, 1975. The investigation showed a severe aplastic anemia with a totally eliminated bone marrow. On November 10, pretreatment was started in order to knock out the patient’s immune system, i.e. prepare him for the graft from his donor brother.
On November 12, the transplant was performed. The donor was anesthetized in the surgical department. Carl-Gustaf Groth and I aspirated bone marrow cells from his hip bone during anesthesia. It took about 4 hours. Göran Lundgren, Carl-Gustav’s right hand as transplant surgeon, took care of the patient and made sure that one liter of donor bone marrow was perfused into the patient’s venous system via a central venous catheter. The following days we worked intensively with the patient. The supportive treatment is very important. However, after a few days, it became apparent that the new bone marrow was being rejected. We had many phone calls with the Mecca of bone marrow transplantation – Fred Hutchinson Cancer Center in Seattle – and their bone marrow transplant group. After a series of attempts to get the donated bone marrow to take, there was no way out other than to make a new transplant after just one and a half months. Now we succeeded better. In March 1976, the patient had a practically normal donor bone marrow. The white blood cells were normal while the platelets improved more slowly. In May, we thought the patient was so well that he could go home. But then he got a pneumonia with the feared Cytomegalovirus. At this time, there was no treatment for this virus and the patient died less than half a year after the first transplant.
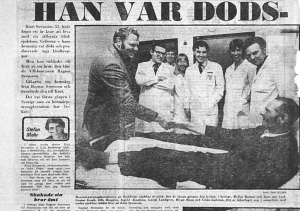
We weren’t ready to re-perform another transplantation attempt until 1977. The patient, a 51-year-old man, had then been referred to us from a hospital in southern Sweden. Like the first patient he also had severe aplastic anemia with bleedings, low hemoglobin content, low platelets, low white blood cells in the peripheral blood and an “empty” bone marrow – all consistent with the diagnosis of aplastic anemia. We first treated him in the usual conventional way with anabolic steroids and prednisolone without any effect. The patient was fortunate to have 6 brothers. Three of these fitted as donors. All the brothers were willing to donate, but the ones who quickly registered themselves were the former Olympic gold medalist in wrestling, Pelle Svensson and his brother Ragnar. On September 1, 1977, the transplant was performed. Everything went as we had hoped. The bone marrow engrafted with marrow from his brother Ragnar who was the only one who was suitable according to HLA typing. The number of white and red blood cells and platelets gradually increased. The common complications of graft-versus host disease and infection occurred but were relatively moderate. On December 9, the patient went home, cured from his severe disease. Both brothers came to newspaper interviews. There was quite a lot of positive attention in the press.
Eventually the successes at Huddinge Hospital became exceptional. Six patients with severe Gaucher disease were transplanted until 1993. The two first transplanted patients live healthy 17 and 20 years after transplantation, respectively.
The bone marrow transplant research at Huddinge Hospital was extremely successful. The allogeneic transplantation activity was high. Between 50 and 70 transplants were performed every year, and were supplemented in the early 1980s with autologous transplants, i.e. transplants with the patient’s own bone marrow. When the results for established indications such as aplastic anemia, acute leukemia and chronic myeloid leukemia proved to be good, , it was time to expand to other disorders. In 1983, Berit Lönnqvist had admitted a woman with therapy resistant multiple myeloma, another life threatening cancer disorder, mainly located to the bone marrow. After the transplant the patient remained without any signs of disease for four years and we thought that we had cured the first patients in the world with this, until now, incurable disease. Although 4 years was an exceptionally long disease free survival time, relapse then occurred. However, the start was taken for a long term international collaboration program about multiple myeloma having resulted in cure of a small fraction of patients.
On the international scene, Huddinge Hospital’s bone marrow transplant group has been quite successful. Much of the activity has taken place in joint projects within the European Group for Blood and Marrow Transplantation (EBMT). This has also meant that many of us have been very active in this organization.
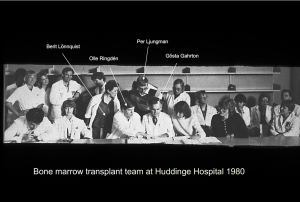
In the early 1980s, I heard a talk about gene therapy. I had not deepened myself on this subject before but became completely fascinated after a lecture and realized that gene therapy would very likely be the weapon one. Bone marrow transplant team at Huddinge Hospital 1980 the future in many hereditary diseases and perhaps also in cancer diseases. However, my conversation with the visitor was somewhat disappointing. He clearly stated that only idiots are dealing with gene therapy, nobody believes that in the foreseeable future it will be useful in the clinic. Eventually, in 1988, reports from the United States revealed that genes had been transferred to cells that had then been transferred to humans. On December 15, 1995, in connection with an autologous transplant to a myeloma patient, we were able to transfer myeloma cells that we had marked with a gene, the idea being to receive information if later recurrences came from given autologous cells or from persistent malignant cells. Out of eight patients two relapsed within a few years and no one had marked myeloma cells indicating that the relapsed cells derived from persistent and not from transplanted ones. This was the first gene transfer clinical trial in Sweden.
However, it was not the hematologists who did the first human treatment attempts with gene transfer in Sweden. The myeloma project was a marking project without treatment aims. Christer Sylvén at the Department of Cardiology started a gene therapy project, with the aim to improve vascularization in the heart after an infarction. By injecting the VEGF (vascular endothelial growth factor) gene directly into the heart improved vascularization could be obtained in the area that was previously the subject of infarction. The trial was ongoing for some years, but was then closed. Sufficient revascularization was not obtained to make the method clinically relevant. Although the gene therapy path has been difficult thousands of projects are ongoing in the world. Recently a successful treatment of cancer – CAR T-cell therapy – is based on gene transfer procedures.
Edvard Smith, at the center for Biotechnology and clinical immunology worked for several years together with me to initiate a gene therapy center. The aim was to produce vectors for genes of interest of high quality. The day before the hospital director was to resign in 1995, I plunged into her office to get her signature on the document. This would ensure the gene therapy center 5 million Swedish crowns per year for four years and then hopefully be self-sufficient. I got the signature and the building could begin. The Gene therapy center is now in place. Without the pioneering spirit that has prevailed in Huddinge hospital during all years, the development from bone marrow to gene therapy had not been possible.
Berit Lönnquist
Olle Ringdén
Per Ljungman
Gösta Gahrton
